


AUTHORS: Eileen F. Morrison* and Colleen Carney Love¡
* Richmond, VA, USA
¡ Atascadero Hospital, Atascadero, CA, USA
Published in the Archives of Psychiatric Nursing
Volume 17, Issue 4 , August 2003 , Pages 146-155.
Copyright © 2003 Elsevier Inc. All rights reserved.
CITATION: Morrison EF, Carney-Love C; An evaluation of four programs for the management of aggression in psychiatric settings. Arch Psychiatr Nurs Aug 2003, 17(4) p146-55.

Regulatory agencies are encouraging health care facilities to address the problem of violence to employees. In response to this pressure, most psychiatric facilities now require and implement formal education for the nursing staff on a yearly or biannual basis in the management of aggressive behavior (MAB). Although some of the programs are good, not all are based on sound professional and clinical principles and very little is publicly known about the results of scientific study of these programs. Our goal with this report is to evaluate several commonly used programs for the management of aggressive behavior using a set of predetermined criteria. Hopefully, this discussion will stimulate a debate over the effectiveness of these programs, and others, that dot the landscape and foster clinical research that examines staff injury rates as well as other common and clinically important patient outcomes, such as violence.

AGGRESSION AND Violence are often cited as a major occupational hazard in health care facilities [Byrnes 2000, Lipscomb and Love 1992 and Rippon 2000]. A survey conducted by the American Nurses Association in 2001 found that 25% of nurses named on the job assault as a great concern; 17% had been physically assaulted in the past year and more than half (57%) were threatened verbally or verbally abused [American Nurses Association 2001]. Attracting the attention of the Office of Health & Safety, injury rates to nurses in public sector psychiatric facilities from violence alone are twice as high as injury rates from all causes reported in traditionally high risk industries [Love and Hunter 1996]. These numbers are surprising, given that no standards exist for measuring and reporting mechanisms in health care, resulting in a gross underreporting of assaults [Lion et al 1981].
The lack of research based violence prevention standards from which to work has left thousands of nurses working in hazardous conditions with few reliable resources at their disposal to prevent and effectively manage violence toward themselves, their coworkers or patients in health care settings. The severity of the problem in psychiatric facilities and consequences of assaults and injuries are well documented. For example, [Love and Hunter 1996] documented staff injury rates in six state psychiatric hospitals that ranged from 11.7 to 16.9 injuries per 100 employees. Aggression and violence is both costly to the institution [Hunter and Carmel 1992] and results in considerable psychological sequella for the staff [Duxbury 1999, Lanza 1984, Lanza 1992, Love and Hunter 1996, Poster and Ryan 1989 and Ryan and Poster 1989]. Nurses assaulted by their patients may experience loss of time from work, financial costs and protracted psychological sequella, including a variety of posttraumatic stress responses. In one study the costs to one hospital for an assault in terms of lost time and legal fees was approximately $250,000 [Hunter and Carmel 1992]. However, despite these consequences for aggression and violence, institutional and individual roadblocks still exist which interfere with the examination of causes of aggression and violence and effective interventions or prevention programs. For example, denial by administrators that violence exists and an attitude that "its part of the job" by the front line staff often perpetuate an unwillingness to address the issue [Lion 1987 and Maier 1999]. A fear of liability may also inhibit administrators from exploring the scope of the problem or from developing effective interventions. The dependent nature of these institutions on the public sector for policy and financial direction contributes to the situation by fostering a status quo or don't rock the boat attitude.
Several interventions for violence have received some, but insufficient attention in the literature: seclusion and restraints [Brooks 1987, Brown and Tooke 1992 and Soloff et al 1985], medications [Corrigan et al 1993], limit setting [Gallop 1990 and Gallop 1993], de-escalation [Morales and Duphorne 1995 and Stevenson 1991], and the need for training [Barile 1982, Carmel and Hunter 1990, Grube 2001, Hurlebaus and Link 1997, Infantino and Musingo 19, Lehman et al 1983, Lion 1987, Martin 1995 and Nigrosh 1983]. Unfortunately, this literature is not often theory or researched based and it does not provide sufficient direction for managing the problem. In most cases, it expresses expert clinical opinion and leaves the question of intervention effectiveness begging.
Because of the scope of the problem, the Office of Safety and Health Administration (OSHA), recommended guidelines for health care facilities to provide education on the management of aggressive behavior. Psychiatric facilities now implement formal education for the nursing staff on a yearly or biannual basis in the management of aggressive behavior (MAB). This need for training has resulted in a small cottage industry of mental health consultants selling a program usually based on some martial arts program. Although some of these programs are excellent, not all are based on sound professional and clinical principles and very little is publicly known about the results of scientific study of these programs. Our goal with this report is to evaluate several commonly used programs for the management of aggressive behavior using a set of predetermined criteria.

Very little literature exists on the topic of training staff for the management of aggressive behavior in psychiatric facilities, which is interesting, considering the importance of the topic. [Lehman et al 1983] first showed that training staff in the prevention of violence, and methods of verbal and physical de-escalation techniques led to improved knowledge about and confidence in handling violent situations. Shortly after, [Infantino and Musingo 19] took the study of training one step forward to measure a specific staff outcome such as, injuries. The results showed that training led to a statistically significant reduction in injuries. By the late 1980s programs for the management of aggressive behavior were already widely in use in the Unites States, when [Lion 1987] added his voice to the literature. Lion advocated that the American Psychiatric Association develop policies and regulate staff education for aggression management; requiring all professionals to attend. Unfortunately Lion used a metaphor to reflect staff-patient relationships, "training for battle" which contributed to an adversarial attitude between staff and patients that continues in some places today.
Two facilities have implemented staff training as part of a long-term program designed to decrease violence in a maximum security, forensic psychiatric facility [Carmel and Hunter 1990, Love and Hunter 1996 and Rice et al 1989]. At Atascadero Hospital in California, violence is viewed as an occupational issue resulting in a "no violence" policy. The problem is addressed using the Quality Improvement Methods specified by [Deming 1986] focusing on staff injury rates. One study from Atascadero showed that units with high staff compliance in training had statistically fewer injuries than units that had low compliance with training [Carmel and Hunter 1990]. But staff with compliance in CPR training also had significantly lower injury rates, suggesting that some aspect of group cohesion or the Hawthorne effect might account for the decrease in injury rates, not training. In contrast, Rice's group approached the problem from a research perspective measuring not only knowledge and confidence levels of staff, but also assaultive levels of patients. The results showed an initial significant reduction in assaults after training, followed by an increase in assaults [Rice et al 1989].
The problem has transcended culture and is now noted in other English-speaking countries such as England, Wales, and Scotland. These countries have their own version of education programs. The United Kingdom just published a report, the first of its kind, on the recognition, prevention and therapeutic management of violence in mental health care [United Kingdom Central Council for Nursing and Midwifery and Health Visiting 2002]. This report summarizes the literature, the results of a survey on practitioners, an analysis of policies on aggression, an analysis of training programs and the results of a consultation exercise. Their main findings on the education and training programs are as follows: programs are widely available, very few attend these programs and no systematic examination of these programs or their trainers have been conducted [United Kingdom Central Council for Nursing and Midwifery and Health Visiting 2002].

When several educational options exist, how is a decision made regarding which program to use? Currently the process is very haphazard and emotionally motivated. Sometimes, the cost to the hospital is the primary criteria. For others, staffs' psychological comfort after training is the criteria for decision-making. This report will provide an example of how clinical decisions can be made using a more systematic and critical process. In this model, clinical decision-making is viewed as a 3-step sequence: search-analyze-choose. The entire process follows these steps: (1) define the overall purpose and goals, (2) define the problem, (3) specify constraints, (4) specify the approach to the problem, (5) state behavioral objectives and performance criteria, (6) list alternative solutions, (7) analyze the options, (8) choose decision rules and (9) implement decisions [Baily and Claus 1975]. This model can be thought of as a precursor to the Continuous Quality Improvement Process used in many hospitals today and can be helpful to nurses when making clinical decisions on interventions.
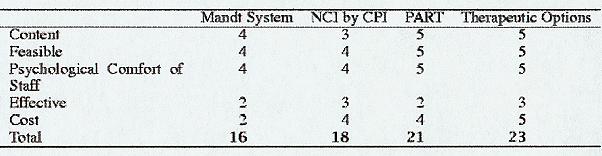
Five criteria were chosen to evaluate the programs: the content, the feasibility, the psychological comfort of the staff, the program's effectiveness, and the cost [Baily and Claus 1975]. The first criteria, content refers to the material covered. Most programs emphasize physical techniques but minimize theoretical considerations. Does the program include unnecessary information and is the information helpful? The feasibility of the program refers to the ease of implementing the program. Are the techniques too complex, i.e., will it require a great deal of training or skill to perform the techniques. The psychological comfort of the staff is shown by their sense of confidence in dealing with aggressive situations after taking the program. The effectiveness of a program is shown by research efforts or by program evaluation data that shows a decrease in clinical outcomes such as seclusion and restraints, patient and staff injuries, or violence. The last criteria are the cost to the institution for the program. Obviously, a high-cost staff member is an institutional barrier to implementation. All criteria except cost were scored on a scale of 1 (not met) to 5 (well met). Cost was reverse coded. The potential range of scores is 5-25; the higher score meets the criteria. Each criterion is equally weighted and the highest score obtained is perceived as the best educational program. The background of the founder should be made public and also considered in an overall evaluation of the program.
The following evaluation is based on (1) the authors combined 15 years of experience working in forensic psychiatric settings and 15 years in psychiatric settings, (2) reading the published literature and the literature provided by the companies on their program, and (3) talking with, observing and supervising staff about their experiences, (4) participating in aggressive situations, and (5) conducting research and studying various aspects of patient violence. A limitation of this evaluation is the amount of information used to evaluate the programs. The manuals for the programs can be extensive and not every program provided a manual for review. In addition, the authors have participated in some of the programs, but not all. As such, the evaluation is based on the authors "expert" opinion that can be accepted or not by the reader. Certainly, readers may disagree with some of the evaluation scores, as did some of the company's representatives in their prepublished reading of the manuscript. What is most important is that the institutional users of these programs ask similar questions about the programs. However, given these limitations, the authors hope that the evaluation provides some direction for users of these programs.

Four programs will be evaluated; The Mandt System [Mandt], Nonviolent Crises Intervention [Crises Prevention Institute Inc. 1987], Professional Assault Response Training [Fox et al 2000] and Therapeutic Options [Partie 2001].

The Mandt System was one of the first aggressive management programs in existence and is widely used in over 45 states [Mandt]. It originated in 1975 in response to the need for training in residential facilities regarding the management of persons with uncooperative or aggressive behavior. The program was extensively revised in January of 2002 and now boasts that the course addresses all regulatory and licensing recommendations.
Mandt is defined both as "a systematic training program designed to help you de-escalate yourself and others when you or they are out of control" and as a "graded system of alternatives for de-escalating people". Out of four stated objectives of the program, three address liability issues. The only theory proposed in the course is the Crises Development Model, but it is acknowledged that the system blends well with a behavior management approach [Mandt].
The content is organized into three levels: basic, intermediate and advanced. The basic level has three modules including: (1) building healthy relationships (working as a team, causes of stress and the crises cycle, understanding emotions), (2) building communication (nonverbal elements in communication, vocal elements in communication and strategies for de-escalation) and (3) conflict resolution and problem solving. The intermediate level has six modules including: (1) building conflict resolution, (2) behavior support, (3) assisting (body mechanics, posture, movement, one and two person physical assisting and supporting holds), (4) separating (holds, releases, biting and hair pulling), physical restraint (standing, moving restraint, falling down, sitting or kneeling restraint, child restraint), and (5) liability and legal issues. The advanced module includes: an introduction to the Mandt System philosophy, the training approach, leadership and quality of care, conflict management and resolution, body movement and mechanics, unarmed attack, armed attack, changing a person's space, and lying down restraint [Mandt].
The Mandt System is a 5-day course (Basic & Intermediate 35-40 hours) that costs $995/person for the initial training. The advanced level is a 4-day program. Recertification is required every 2 years at a cost of $695 plus travel to the site and per diem. In the past, trainers could adapt the program, but trainers are no longer allowed to make any changes to the programs. Trainers teach a 1-day course in their facility that is required for staff yearly.
Although the Mandt System representatives claim that in program evaluations participants report that they are comfortable with the program, in facilities known to the authors that use the Mandt system staff are highly critical of the program. The company also claimed that a 90% reduction in restraints and seclusion in Pennsylvania supported the effectiveness of their program. But the overall improvement in restraint use in Pennsylvania was because of a large variety of programs, including Mandt.
Although the basic level is quite similar in the revised version, the inclusion of conflict resolution and problem solving techniques is a major improvement. Second, the inclusion of liability and legal issues in the intermediate level also adds to the programs viability by helping staff to understand some of the consequences for their negative behavior towards patients.
Several limitations to the program also exist. First, an explicit idea underlying the philosophy is that someone is out of control, which is not necessarily the case [Morrison 2001, Morrison 1992a, Morrison 1993 and Morrison 1993]. Although the relationship of violence and schizophrenia is inconclusive, violence by the mentally ill is decidedly more predatory and co-occurs with substance abuse and criminal justice histories. This profile of violence as predatory suggests that individuals use their behavior in an intimidating and exploiting manner to frighten others into complying with stated requests. This aspect of violence is only likely to get worse in the future and must be better understood [Morrison 2001]. Any program aimed at preventing or managing violence must address the predatory aspect to be effective.
A second theoretical limitation of the Mandt System is the importance given to the possibility that staff is out of control. It is true that sometimes staff provoke patients [Morrison 1992b]. The Mandt System manual states that attempting to control others by gaining compliance is a leading cause of violence. The company argues that this idea is based on Bandura's concept of intrinsic motivation. The authors disagree only in how to manage the situation. By the time a staff member is de-escalated, you might have a patient abuse situation. When provocation occurs, you do not wait to de-escalate staff! Any competent staff member should step in and tactfully remove the staff member from the situation as soon as possible. The staff member and patient can then be safely dealt with individually and in private. In any case, we doubt that Bandura would argue that staff are "out of control"; only that staff have some compelling negative motivations.
The last limitation of the Mandt System is the obvious lack of education focused on behavioral principles which are now accepted as the cornerstone of treatment and which are insufficiently taught in most nursing education systems. However, the new version of the program is more clearly based on Bandura's understanding of how people acquire skills and includes more information on behavioral principles; a decided improvement [Bandura 1971]. Thus, The Mandt System scores are 4 for content, 4 for feasibility, 4 for comfort of staff, 2 for effectiveness and 2 for cost. The lack of sound evaluation data and the high cost for this system reduce the score significantly (total = 16; Table 1).


The second program widely used for the management of aggressive behavior is distributed by the Crises Prevention Institute [Crises Prevention Institute Inc. 1987]: Nonviolent Crises Intervention. NCI, a practical approach for managing violent behavior is probably the most aggressively marketed program available in the US, UK, and Australia (www.crisesprevention.com) and boasts training over 3.5 million providers since 1980s. CPI does maintain contact with their instructors and provide a fair amount of opportunities for continuing education for instructors, through the web, newsletters, testing, and workshops. The newsletter is particularly good and provides updates from successful hospitals and important information on related topics such as seclusion and restraints. The web site boasts that NCI "is considered to be the worldwide standard for the safe management of out of control behavior" (p. 1). The basis of this claim is not justified. Although most of the company's are interested in establishing educational standards, to the author's knowledge no standard currently exists.
The course content has three sections: (1) prevention techniques, (2) team approach and therapeutic physical intervention and (3) postintervention. A nice description of a verbal de-escalation continuum is included with verbal intervention do's and don'ts as well as the importance of empathic listening. Insufficient time in this module is spent on clarifying precipitating factors, whereas too much time is spent on staff fear, anxiety, and self-control. Prevention techniques include: nonverbal techniques such as empathic listening, and verbal techniques. Therapeutic physical intervention includes safety techniques to protect oneself from injury as well as team therapeutic physical intervention techniques. Examples of safety techniques are: a kick block, wrist grab release, hair pull release, choke release and bite release. Examples of team therapeutic physical intervention techniques include: control position (adult and child, interim) and transport techniques. Although the program does not include evasive techniques, a series of releases from holds are included helping staff indirectly to feel less fearful in aggressive situations. The manual is written in outline format with room for note taking. Pictures of holds are included [Crises Prevention Institute Inc. 1987].
Certification is a 4-day course that costs $995/person plus travel to the training site. Recertification is required every 4 years and costs $395 for a 3-day course, making this a bit cheaper than the Mandt System. Instructors are allowed to teach either a 1-day or 2-day workshop for their staff and are not allowed to change or adapt the course. The course content has changed very little since its inception in the 1970s. A variety of smaller fees are included for yearly on line testing and recertification. Attendees are only briefly encouraged to examine the precipitating factors for acting out behavior, missing an important theoretical piece of the problem solving in any aggressive situation. The last section, the postintervention is poorly developed and described, but encourages staff to review the situation after its conclusion to learn from it. Although this section is a nice addition, resources are available elsewhere for Critical Incident Debriefing and probably more time is required to teach staff its proper use. The acronym COPING is used to focus staff on different aspects of the situation: c for control, o for orientation, p for patient patterns, i for investigation of alternatives, n for negotiation of alternatives, and g for give staff feedback. The use of the acronym makes it easier to remember.
The company provided some evaluation data, which provides information on staff comfort and feasibility of the program, but not for program effectiveness. First, CPI conducted a survey of 8,000 instructors. One thousand were returned, i.e., a 12.5% return rate. Eighty percent of those returned reported a perceived reduction in assaultive incidents, 75% reported a perceived decrease in Worker's Compensation and 77% reported a perceived reduction in disruptive incidents. An increase in staff confidence was observed by 98% instructors and 86% reported an improvement in staff morale. Second and more importantly, two publications exist with evaluation data [Jambunathan and Bellaire 1996]. Summitt State Hospital instituted a comprehensive restraint reduction program, including NCI, which showed a significant reduction in restraints; from 1,132 in 1998 to 4 in 2,000. Arizona State Hospital also implemented NCI training for its staff and recorded the number of staff who were struck before and after training. Before NCI training 31.5 strikes/month occurred, while after training the number reduced to 18.2 strikes/month (1998). Again, when examining staff perceptions of situations, [Jambunathan and Bellaire 1996] reported that staff perceived resolution of crises in 84% of the episodes after training in NCI. Several articles in the CPI newsletter provided seclusion and restraint data in several sites to show significant reductions [Crises Prevention Institute Inc. 1987].
To summarize the major points, (1) the content is insufficient for managing today's violence, (2) it is an expensive program for hospital users, (3) the lack of sufficient evaluation data and (4) the positive inclusion of data on staff's comfort with implementation of the program. Thus, the scores for NCI are 3 for content, 4 for feasibility, 4 for comfort of staff, 3 for effectiveness, and 4 for cost (total = 18).

The third program, developed by Paul Smith is the most well developed program reviewed [Fox et al 2000]. PART 2000 is in wide use in California and has been adopted for use in Germany and Australia. It has gone through several revisions as a result of clinical experience with the program and the reasons for changes are clearly documented in the packet.
PART emphasizes the use of a systematic approach, rather than a variety of techniques, to teach participants critical thinking and problem solving skills to apply in any situation. A basic premise is that employees who have developed a systematic approach are less likely to get injured than those relying on a variety of techniques. PART also emphasizes that the program is to be used in conjunction with the professional treatment team's plan for the patient and used only after the failure of the intervention plan and the back up plan when an immediate threat of injury exists [Fox et al 2000].
The content is organized into eight chapters. The first chapter of PART focuses on developing patient assessment techniques, while chapter 2 focuses on professionalism by examining key psychological aspects of the staff. Chapter 3 is based on preparation; attire, mobility, observation with a lengthy section on the importance of maintaining staff self-control that is particularly strong. Chapter 4 is a key chapter and covers identifying triggers and alternatives by reviewing the underlying theories: a stress model of assault, developmental theory, Maslow's hierarchy of needs and communication theory. If a critique can be made of this chapter it is that it strives to do too much and the most useful points are lost, however, the material is clinically justified. Environmental triggers that stimulate violence are also discussed. Chapter 5 includes useful information no other program does, i.e., levels of dangerousness, what is reasonable force and how is it used and the use of matching crises communication to the level of injury threatened. The Common Knowledge Model is presented in chapter 5 and makes explicit the reasons why patients are aggressive: fear, frustration, manipulation and intimidation. Although arguments can be made about frustration as a cause for aggression, the identification of manipulation and intimidation as reasons for violence is exceptionally timely and is the only program to include this information, a significant advantage. Chapter 6 is solely focused on teaching evasion techniques. It is really surprising that something so simple and helpful is omitted in many of the other programs. Chapter 7 focuses on seclusion, restraint, and pharmacologic interventions. The physical exercises in this program are all designed to be used by teams of staff members; a more realistic approach. The last chapter is focused on the importance of recording in the formal document of what occurred [Fox et al 2000].
PART is a 5-day course costing $650/person, plus travel for training. A PART Instructor will come to your facility to teach 16 staff for a cost of $6,250 plus expenses. Recertification is required every 3 years and costs $360 for 21/2 days training, making this program a bargain compared with other programs. Trainers then provide their employees a 2-day course requiring more time than other programs. PART is used most by the state of California, but has about 25 training sessions/year. Because of its many positive aspects, PART has been recognized by JCAHO, CAL-OSHA, ACDD, and a variety of other regulatory and licensing agencies.
PART has a lot of points to recommend it including the following. First, the theoretical content is up to date and current with interdisciplinary treatment planning. Second, it includes a nice description of legal terms and responsibilities. Third, the focus is on team interventions. Fourth, the use of decision trees, which were developed for responding to self-injurious behavior suggesting alternative behaviors, using crises interventions, principles of evasion and finally the use of manual restraint make the process easy to follow. The inclusion of intimidation and manipulation as a cause of violence is a particularly strong part of the program.
The program has not been formally evaluated by an examination of clinical outcome measures. However, during the use of the program and the subsequent informal evaluation, several discoveries were made. First, the trainers often changed programs and sometimes techniques that were not considered standard professional practice were included. This is likely a common problem with all the programs. Second, standard martial arts were sometimes substituted for the program. Third, language influenced behavior, i.e., the use of the term takedown led to the use of physical restraint as a first measure, not a last measure. Staff in facilities that use this program seem very satisfied with its use.
To summarize, the advantages and disadvantages of PART are: (1) strong theoretical approach and the inclusion of intimidation, (2) the inclusion of evasion techniques, (3) the use of team techniques, (4) inexpensive cost, (5) inclusion of staff liability, and (6) limited evaluation data. Thus, the scores for PART are 5 for content, 5 for feasibility, 5 for comfort of staff, 2 for effectiveness, and 4 for cost. The lack of sound evaluation data is the only important limitation of this program (total SCORE = 21).

TO is a "comprehensive and sensible approach to reducing violence and the use of restraint and seclusion in behavioral health care" [Partie 2001]; www.therops.com. The philosophy of TO is well developed and is based more closely on the issues identified in the literature as important. TO emphasizes the therapeutic relationship and the need to support alternative adaptive skills, rather than violence. One goal is the achievement of a violence free therapeutic environment with a decreased reliance on physical intervention skills when it does occur. The program includes a nice description of how institutions rob patients of their dignity and self-respect and the importance of giving them a sense of self-determination, tying the program into the literature for de-deinstitutionalization [Partie 2001].
The program is clearly based on positive behavioral support and employs the concepts and methods of applied behavioral analysis within a person centered approach. A functional model of behavior assessment and change is taught in which all behavior is viewed as functional for the person. Although some material on self-awareness is included, the emphasis is more on managing stress and supporting others in a difficult situation. The founder, Michael Partie, is a social worker and a behavior specialist with extensive experience working in institutions as well as community settings with children and adults. He was also the Chief Patient Abuse Investigator for a state system indicating that he understands the "other side of the coin."
In contrast to some programs, the manual has a great deal of information and can serve as an excellent resource after the course. Some programs only provide an outline of the material in the manuals with space for taking notes. The TO manual has a long section on the therapeutic relationship and behavioral principles . Although the material is theoretical, it has a large number of very useful and pragmatic examples, making it easy to read and applicable to practice. A nice section is included with a full description of the crises cycle with examples of how the helper intervenes. Of all the programs, TO did the best job with this material [Partie 2001].
Therapeutic Options Inc. offers other courses such as Psychiatric Rehabilitation and Recovery and Investigating Critical Incidents demonstrating their commitment to the use of the interpersonal therapeutic relationship and the use of examining clinical outcomes. In the rehabilitation course, the following are included: (1) connecting skills, (2) assessing readiness to change, (3) developing readiness for change, (4) setting a goal, and (5) team process and person centered planning.
As part of the evaluation efforts of a large residential habilitation center, evaluation data was monitored after TO on assaults and injuries. One year after training: a 36% decrease in injuries, 70% decrease in assaults, 48% decrease in work time lost, and a 50% decrease in back injuries were reported. Although the implementation of the TO program was only one part of a comprehensive program to increase staff safety and client safety, the clinical and administrative staff give TO the informal credit for a major part of the improvements. The TO certification course is 5 days in which the trainer comes to the facility at a cost of $5,000, plus expenses for training 14 staff members. While the initial financial investment is high, the long-term cost is relatively inexpensive if training 14 staff. Recertification occurs every 2 years for 2 days at a cost of $2,000 plus expenses ($143/person).
To summarize, the advantages of this program include: (1) a well developed philosophy, (2) a strong component addressing the therapeutic relationship and an understanding of power relationships, (3) a strong behavioral component, (4) closely linked to current literature base, (5) relatively inexpensive, and (6) examines the effectiveness through clinical outcome data. Thus, the scores for Therapeutic Options are 5 for content, 5 for feasibility, 5 for comfort of staff, 3 for effectiveness and 5 for cost (total = 23).

Although all the programs have limitations, a comparison of the overall scores on the programs suggests that TO (23) and PART (21) have the highest scores. Their content is better than the other programs, the staff feel more comfortable using these programs and the cost is lower for the institution. The newest version of Mandt is a big improvement over older versions and will need time to see if staff are more comfortable using it or if it is more easily used and CPI is quite outdated. TO is the cheapest for training a large number of staff.
The early programs were developed by applying some martial arts defense program and relied almost exclusively on physical techniques of self-defense. More recently, programs are trying to address the idea that staff "are trying to make patients do what I want." Newer programs have more depth and breadth, address what is recommended by regulatory agencies, and include some of the newer theoretical and therapeutic principles. Most need a stronger theoretical component, especially with respect to behavioral assessment and principles and how staff can unknowingly reinforce violent behavior through rewards. It is interesting that not one of the programs introduces any nursing research to support their program. Only PART 2000 introduces the idea of treatment planning and how the management of aggressive behavior program fits into the overall treatment plan and is the only program that introduces evasion techniques. Only TO acknowledges the importance of having a therapeutic relationship with the patient and describes how this relationship differs from other relationships. All the programs are taught using a wide variety of teaching techniques: lecture, discussion, role play, demonstration, and so on.
Some general criticisms of these programs can be made. First, most assume that the patient is cooperating when in reality most are resisting or actively fighting. Second, team techniques are not sufficiently covered, especially since [Carmel and Hunter 1990] showed that group cohesion may be an important factor in reducing injuries. Two of the programs (PART 2000 and TO) are used in systems that have an overall long-term plan or quality improvement program designed to reduce violence. As part of this program, statistics on injuries and violence are kept and monitored for any improvements. Tracking changes in rates should be an integral part of any hospitals monitoring system. User survey's done on behalf of the program, are insufficient evaluation data since surveys only measure how staff perceive an event and sometimes this has no relation to the true incidence of the event.
Violence should be addressed with a comprehensive program and viewed as an "occupational problem requiring a cohesive, multifaceted organizational approach" [United Kingdom Central Council for Nursing and Midwifery and Health Visiting 2002]. This approach should include a "no violence" policy, a systematic measurement system, comprehensive CQI program, a Critical Incident Stress Debriefing Program and support for filing charges.
A primary concern with respect to these programs has been the lack of clinical standards on the teaching of the management of aggressive behavior. In 1983, Nigrosh first pointed out that we only had to follow the very successful precedent set in cardiopulmonary for CPR education. However, it was not until 2002, when the United Kingdom published the first standards for the education of managing assaultive behavior [United Kingdom Central Council for Nursing and Midwifery and Health Visiting 2002]. At the least, these programs should include the following: (1) the use of the overall treatment program and the therapeutic relationship as the overall context, (2) behavioral theories and functional assessments, (3) the necessity for staff to maintain control, (4) legal concepts & issues of patient abuse, (5) pharmacologic treatment of violence, (6) review of alternative interventions, (7) team physical techniques (evasive techniques, breaking free, immobilizing, and transporting patients) for patients who are noncooperative, (8) restraining patients with certain medical conditions, (9) restraining children and elderly, (10) movement in and out of seclusion, (11) risk of restraints and (12) medicating a noncooperative patient. In addition, specific physical techniques need to be researched and standardized to minimize injuries of staff and patients. The ergonomic nature of physical holds needs to be examined to ensure physical safety for staff.
Aggression and violence are no longer questioned as important clinical issues in psychiatric settings. Despite the general consensus of this idea, we do not seem to be making any significant progress towards finding solutions or even effective interventions aimed at protecting staff when at work. Some of the consequences of staff assault are clear. Staff injuries are expensive and result in a traumatized staff member who may not function well at work for quite awhile. Hospitals incur a considerable yearly cost for the training of staff in programs for the management of aggressive behavior. Although these programs undoubtedly help staff to feel better about managing aggressive patients, the question must be asked "do they work?" The answer to this question is not yet clear. This article has made one step forward toward evaluating four of these programs in the hope that other evaluative efforts will occur and eventually stimulate research and the establishment of clinical standards.

American Nurses Association 2001. American Nurses Association. Nursing World website. On Line Health & Safety Survey; ANA (2001).
Barile 1982. L.A. Barile, A model for teaching management of disturbed behavior. Journal of Psychosocial Nursing and Mental Health Services 20 11 (1982), pp. 9-11.
Baily and Claus 1975. J. Baily and K.A. Claus. Decision making in nursing: Tools for change, The C.V. Mosby Co, Saint Louis (1975).
Bandura 1971. A. Bandura. Aggression: A social learning approach, Prentice-Hall, Englewood Cliffs, NJ (1971).
Brooks 1987. M. Brooks, Control and restraint techniques: A study of their effectiveness at Gartee Prison. Prison Service Journal (1987), pp. 11-13 October.
Brown and Tooke 1992. J. Brown and J. Tooke, On the seclusion of psychiatric patients. Social Science and Medicine 35 4 (1992), pp. 711-721.
Byrnes 2000. J.D. Byrnes, The aggression continuum: A paradigm shift. Occupational Health & Safety 69 2 (2000), pp. 70-71.
Carmel and Hunter 1990. H. Carmel and M. Hunter, Compliance with training in managing behavior and injuries from inpatient violence. Hospital and Community Psychiatry (1990), pp. 558-560.
Crises Prevention Institute Inc. 1987. Crises Prevention Institute Inc.. Nonviolent Crises Intervention Training Program: Instructor's Manual (1987) CPI (800-558-8976; Available at www.crisesprevention.com) .
Corrigan et al 1993. P.W. Corrigan, S.C. Yudofsky and J.M. Silver, Pharmacological and behavioral treatments for aggressive psychiatric inpatients. Hospital & Community Psychiatry 44 2 (1993), pp. 125-133.
Deming 1986. W.E. Deming. Out of the Crises, Institute of Technology Center for Advanced Engineering Studies, Cambridge, MA (1986).
Duxbury 1999. J. Duxbury, An exploratory account of registered nurses' experience of patient aggression in both mental health and general nursing settings. Journal of Psychiatric and Mental Health Nursing 6 2 (1999), pp. 107-114.
Fox et al 2000. L. Fox, L. Johnson, M. Nihart, M. Schindler, P. Smith and N. Smiar. Professional Assault Response Training 2000 (2000) California. (949-498-3529, Available at www.part.com) .
Gallop 1990. R. Gallop, The expressed empathy of psychiatric nursing staff. The Canadian Journal of Nursing Research 22 3 (1990), pp. 7-18.
Gallop 1993. R. Gallop, Nurses confirming/disconfirming responses to patient diagnosed with borderline personality disorder. Archives of Psychiatric Nursing 7 6 (1993), pp. 336-341.
Grube 2001. M. Grube, Aggressive behavior in psychiatric patients. Possible modification by self-defense training. Nervenartz 72 11 (2001), pp. 307-311.
Hunter and Carmel 1992. M. Hunter and H. Carmel, The cost of staff injuries from inpatient violence. Hospital and Community Psychiatry 43 (1992), pp. 219-227.
Hurlebaus and Link 1997. A.E. Hurlebaus and S. Link, The effects of an aggressive behavior management program on nurses' levels of knowledge, confidence and safety. Journal of Nursing Staff Development (1997), pp. 260-264 September/October .
Infantino and Musingo 19. Infantino, J.A., & Musingo, S. (19). Assaults and injuries among staff with and without training in aggression control techniques. Hospital and Community Psychiatry Jambunathan and Bellaire 1996. J. Jambunathan and K. Bellaire, Evaluating staff use of crises prevention intervention techniques: A pilot study. Issues in Mental Health Nursing 17 6 (1996), pp. 541-558.
Lanza 1984. M.L. Lanza, A follow-up study of nurses reactions to physical assault. Hospital and Community Psychiatry 35 5 (1984), pp. 492-494.
Lanza 1992. M. Lanza, Nurses as patient assault victims: An update, synthesis and recommendations. Archives of Psychiatric Nursing 6 (1992), pp. 163-171.
Lehman et al 1983. L.S. Lehman, M. Padilla, S. Clark and S. Loucks, Training personnel in the prevention and management of violent behavior. Hospital and Community Psychiatry 34 (1983), pp. 40-43.
Lion 1987. J.R. Lion, Training for battle: Thoughts on managing aggressive patients. Hospital and Community Psychiatry 38 8 (1987), pp. 882-884.
Lion et al 1981. J. Lion, W. Snyder and G.L. Merrill, Underreporting of assaults on staff in a state hospital. Hospital & Community Psychiatry 32 7 (1981), pp. 497-498.
Lipscomb and Love 1992. J.A. Lipscomb and C.C. Love, Violence toward heal care workers: An emerging occupational hazard. American Association of Occupational Health Nursing 34 5 (1992), pp. 000-000.
Love and Hunter 1996. C.C. Love and M.E. Hunter, Violence in public sector psychiatric hospitals: bench marking nursing staff injury rates. Journal of Psychosocial Nursing 34 5 (1996).
Maier 1999. G. Maier, The aggressive patient/inmate: Beyond denial. Psychiatric Quarterly 70 3 (1999), pp. 199-200.
Mandt. Mandt & Associates. The Mandt System: Putting people first. Richardson, TX (972-495-0755; Available at www.mandtsystem.com) Martin 1995. K.H. Martin, Improving staff safety through an aggression management program. Archives of Psychiatric Nursing 9 4 (1995), pp. 211-215.
Morales and Duphorne 1995. E. Morales and P. Duphorne, Least restrictive measures: Alternatives to four point restraints and seclusion. Journal of Psychosocial Nursing 33 10 (1995), pp. 13-16.
Morrison 1992a. E.F. Morrison, A coercive interactional style as an antecedent to aggression and violence in psychiatric inpatients. Research in Nursing and Health 15 (1992), pp. 421-431.
Morrison 1992b. E.F. Morrison, The Tradition of Toughness. IMAGE 20 4 (1992), pp. 222-234.
Morrison 1993. E.F. Morrison, Violence and the mentally ill: Theories, treatment approaches and policy recommendations. In: Violence: nursing debates the issues, AAN, Washington, DC (1993).
Morrison 1993. E.F. Morrison, Towards a better understanding of violence in psychiatric settings: Debunking the myths. Archives of Psychiatric Nursing 7 6 (1993), pp. 328-335.
Morrison 2001. E.F. Morrison, Lessons learned from the trenches about violence. Archives of Psychiatric Nursing 15 2 (2001), pp. 51-52. Nigrosh 1983. B. Nigrosh, Physical contact skills in specialized training for the training for the prevention and management of violence. In: J.R. Lion and W.H. Reid, Editors, Assaults within psychiatric facilities, Grune & Stratton, New York (1983).
Partie 2001. M. Partie. Therapeutic Options Instructor Manual, Therapeutic Options, Newark, DE (2001) (302-753-7115; Available at www.therops.com) .
Poster and Ryan 1989. E. Poster and J.A. Ryan, Nurses attitudes toward physical assault by patients. Archives of Psychiatric Nursing 3 6 (1989), pp. 315-322.
Rice et al 1989. M.E. Rice, G.T. Harris, G.W. Varney and V.L. Quinsey. Violence in institutions: Understanding, prevention and control, Hogrefe & Huber Pub, Toronto (1989).
Rippon 2000. T.J. Rippon, Aggression and violence in health care profession. Journal of Advanced Nursing 31 2 (2000), pp. 452-460.
Ryan and Poster 1989. J. Ryan and E.C. Poster, The assaulted nurse: Short term and long term responses. Archives of Psychiatric Nursing 3 6 (1989), pp. 323-331.
Soloff et al 1985. P.H. Soloff, T. Gutheil and D. Wexler, Seclusion and restraint: A review and update. Hospital and Community Psychiatry 36 (1985), pp. 652-657.
Stevenson 1991. S. Stevenson, Heading off violence with verbal de-escalation. Journal of Psychosocial Nursing 29 9 (1991), pp. 6-10.
United Kingdom Central Council for Nursing and Midwifery and Health Visiting 2002. United Kingdom Central Council for Nursing, Midwifery and Health Visiting. The recognition, prevention and therapeutic management of violence in mental health care, UKCC, London, England (2002).

Harris and Morrison 1995. D. Harris and E.F. Morrison, Managing violence without coercion. Archives of Psychiatric Nursing 9 4 (1995), pp. 203-210.

Corresponding author Address reprint request to Eileen Morrison, PhD, RN,
4010 Hanover Avenue, Richmond, VA 23221, USA.


 Email Charly at: c-d-miller@neb.rr.com
Email Charly at: c-d-miller@neb.rr.com